ten truths (you should know) about ME …
I am stuck in bed, again, and I thought to myself, what is it I would want you to know about ME …
And so below I will document ten things that I think everyone needs to know about ME …
. . . ten truths . . .
. . . you should know about . . .
. . . ME . . .
#1 : ME is a real physical condition …
Many people, doctors included, claim ME is in the mind and then treat people / patients accordingly, which can have a devastating impact on the relationships / friendships or the doctor / patient relationship and will most certainly affect our, as in person with ME/CFS, mental health. Subsequently leaving many of us feeling medically gaslighted and with medically induced PTSD.
FYI — the World Health Organization (WHO) classifies CFS/ME as a neurological illness (G93.3).
neurological:
relating to the anatomy, functions, and organic disorders of nerves and the nervous system …
FYI — NICE state that ME/CFS, which is estimated to affect over 250,000 people in England and Wales, is a complex, multi-system, chronic medical condition where there is no ‘one size fits all’ approach to managing symptoms. CFS/ME comprises a range of symptoms that includes fatigue, malaise, headaches, sleep disturbances, difficulties with concentration and muscle pain. The physical symptoms can be as disabling as multiple sclerosis, systemic lupus erythematosus, rheumatoid arthritis, congestive heart failure and other chronic conditions. CFS/ME places a substantial burden on people with the condition, their families and carers, and hence on society.
So really, how on earth can a GP, consultant, or other professional, get away with claiming otherwise.
#2 : symptoms are much more that just being tired …
Many believe that ME is simply feeling or being tired.
all I can say is:
… if only …
FIY — M.E. is diagnosed following a significant reduction in pre-illness activity levels and an inability to return to normal function. The most important diagnostic symptoms are:
-
- Post -exertional malaise/symptom exacerbation (PEM) (see below) – often with a delayed impact, lasting days or weeks before function is restored. PEM can also trigger a relapse;
- Activity-induced muscle fatigue precipitated by trivially small exertion (physical or mental) relative to the patient’s previous activity tolerance;
- Cognitive dysfunction – problems with short-term memory, concentration, word-finding;
- Sleep problems – sleeping too little or too much, vivid-dreams, unrefreshing sleep;
- Ongoing flu-like symptoms – including sore throats and enlarged glands, fever-like sweats, lethargy;
- Orthostatic intolerance – problems with pulse and blood pressure control leading to feeling faint/dizzy when upright.
Other common symptoms include:
-
- Pain – which can involve muscle, joints and nerves,
- Problems with balance and with temperature control,
- Sensitivity to light and sound,
- Alcohol intolerance,
- Gastrointestinal symptoms.
If you can just go over those symptoms again, slowly, and imagine what having just one of them might feel like let alone all of them.
These symptoms are accepted and used for diagnostic criteria. Sometimes by those medical professionals who refuse to accept th3 illness is physical. GO FIGURE …
#3 : symptom & severity fluctuate …
As if the symptoms alone aren’t enough, but somehow they can fluctuate too. Even worse still, the actual sufferer cannot predict when / why / how … and so, living with these fluctuations can be a logistical nightmare.
When I first got sick, in 1984, I was severe for around six months, followed by a very long period of mild. Then around 1997, after my second child, I became more moderate than severe and for the next 18 years I flitted between mildly moderate to severely moderate. Then I stayed at the worse end of moderate and now, for around five years or more, I’ve been severe and some days I’m severe severe. It is important to point out that even within this severe category I can have better days than others. Some days I’m very poorly, and other days im so unwell I wonder how I am still alive, because I actually feel as though I am dying.
FYI — The ME Association designed a disability assessment scale (see below) that can be useful for following progress and providing information for benefit, employment and insurance assessments.
VERY SEVERE
100% DISABLED: Severe symptoms – often on a continual basis. Cognitive function (i.e. short-term memory, concentration, attention span) is likely to be very poor. Bedridden and incapable of living independently. Requires a great deal of supervision and practical support – including disability aids such as a hoist or a stair lift – with all aspects of personal care (i.e. feeding, dressing, washing) on a 24-hour basis.
90% DISABLED: Severe symptoms, often including marked cognitive dysfunction, for much or all of the time. Bedridden and housebound for much or all of the time. Has considerable difficulties with all aspects of personal care. Unable to plan or prepare meals. Requires practical support and supervision on a 24-hour basis.
SEVERE
80% DISABLED: Moderate to severe symptoms for most or all of the time. Only able to carry out a very limited range of physical activities relating to personal care without help. Requires help with meal planning and preparation. Frequently unable to leave the house and may be confined to a wheelchair when up, or spends much of the day in bed. Unable to concentrate for more than short periods of time. Usually requires daytime and night-time supervision.
70% DISABLED: Moderate to severe symptoms for most or all of the time. Confined to the house for much or all of the time. Normally requires help with various aspects of personal care and meal planning and preparation, possibly on a 24-hour basis. Very limited mobility. May require wheelchair assistance.
MODERATE
60% DISABLED: Moderate symptoms for much or all of the time. Significant symptom exacerbation follows mental or physical exertion. Not usually confined to the house but has significant restrictions on mobility when outside and may require wheelchair assistance. Likely to require help with aspects of personal care and meal preparation – but not necessarily on a full-time basis. Requires regular rest periods during the day. Unable to resume any meaningful regular employment or education.
50% DISABLED: Moderate symptoms for much or all of the time. Symptom exacerbation follows mental or physical exertion. Not usually confined to the house but mobility restricted to walking up to a few hundred yards at best. May require help with some aspects of personal care. May require help with meal planning and preparation. Requires regular rest periods during the day. Able to carry out light activities (i.e. housework, desk work) linked to normal daily living for short periods but not able to resume regular employment or education.
40% DISABLED: Moderate symptoms for some or much of the time. Normally able to carry out most activities linked to personal care and normal daily living, but may require assistance with meal preparation. May be able to cope with some work-related tasks for short periods – provided they are not mentally or physically strenuous – but not able to resume regular work or education.
MODERATE TO MILD
30% DISABLED: Fluctuating level of mild to moderate symptoms. Normally able to carry out all aspects of personal care and to plan and prepare meals. Able to walk short distances on a regular basis. May be able to return to work on a flexible or part-time basis – provided adjustments are made to cope with physical activity or cognitive problems. May have to stop leisure or social pursuits to resume work or education.
20% DISABLED: Normally only mild symptoms at rest but exacerbation will follow activity. Able to carry out all aspects of personal care and to plan and prepare meals. Able to walk short to medium distances (i.e. up to half a mile) on a regular basis. Normally able to return to flexible or part-time work or education.
10% DISABLED: Generally well with only occasional mild symptoms. No problems with personal care or daily living. Mobility and cognitive functions may still be restricted but almost back to previous levels. May be able to return to full-time work or education.
0% DISABLED: Fit and well for at least the past three months. No symptoms at rest or after exertion. Capable of full-time work or education.
#4 : PEM is the signature symptom …
PEM is the signature symptom that appears to be unique to ME.
The more you do … the worse you feel …
There is no other illness, except mitochondrial illness, that is impacted by activity in this way.
FYI — for those who are reading and don’t know what PEM is:
CDC : post exertional malaise (PEM):
Post exertional malaise (PEM) is the worsening of symptoms following even minor physical or mental exertion, with symptoms typically worsening 12 to 48 hours after activity and lasting for days or even weeks. PEM can be mitigated by activity management (pacing).ME Association : post exertional malaise (PEM):
Post-exertional malaise (PEM) is a delayed worsening of symptoms that occurs after minimal physical or mental activity.
It has also been called ‘Post-exertional neuroimmune exhaustion’ (PENE).
The key feature of PEM is that the malaise (extreme fatigue and flu-like symptoms) and other symptoms experienced are not in proportion to the amount of activity that has been done.
PEM is often delayed and may be experienced hours or days after the activity took place but is most likely to occur 1-2 days after the exertion event (Hotlzman et al., 2019).
This delay can lead clinicians and patients to believe that symptom exacerbations are random and unrelated to a trigger as they do not attribute their worsened condition to something that may have happened days earlier.
The effects of PEM can last for hours, days, weeks or even months. Prolonged periods of PEM are often referred to as ‘crashes’ by patients and PEM can even trigger relapse.
The exact cause and mechanisms of PEM are not yet fully understood, though a simple explanation might be that it occurs when a person with ME/CFS has gone outside of their ‘energy envelope’.
This energy envelope is described as the amount a person can safely do without triggering an increase in symptoms and/or symptom severity. PEM is triggered when available energy has been expended and they have gone into ‘energy debt’.
PEM is one of the main features that sets ME/CFS apart from other diseases and explains why exercise can be very damaging in ME/CFS, setting patients back for days, weeks or months.
#5 : there are NO treatments …
Treatments would be really nice to have.
But sadly, as yet, there are no specific treatments for ME, except pacing (see below), which is not really technically a treatment. Think of it more in terms of a self management technique.
Maybe, if you are fortunate enough to have a decent doctor they will treat your symptoms as and when you get them.
Pacing, however, remains the greatest and most successful tool available to us …
Action for ME : pacing:
Pacing is a self-management tool. It is a technique to help you take control of the balance of activity and rest, and learn how to communicate to other people about the balance that usually works best for you.
#6 : genuine specialist clinics are rare …
According to the nice guidelines a person with ME should have a referral to specialist CFS/ME:
— within 6 months of presentation to people with mild CFS/ME,
— within 3–4 months of presentation to people with moderate CFS/ME symptoms,
— immediately to people with severe CFS/ME symptoms.
This would be absolutely wonderful.
However, in practice there are too few specialist ME clinics and in my own case the only specialist I have seen in one I have had to pay for out of my none existent income.
#7 : ME impacts life functionality …
I think I will let the experts speak on this one:
In my experience, (ME/CFS) is one of the most disabling diseases that I care for, far exceeding HIV disease except for the terminal stages. — Dr Daniel Peterson
I split my clinical time between the two illnesses, and I can tell you if I had to choose between the two illnesses [in 2009] I would rather have H.I.V. But C.F.S., which impacts a million people in the United States alone, has had a small fraction of the research dollars directed towards it. — Dr Nancy Klimas
We see cardiac diastolic dysfunction in almost every case … there are patients whose diastolic dysfunction is so low / poor that they would fit well into a cardiac ward awaiting transplant …
The whole idea that you can take a disease like this [M.E./Chronic Fatigue Syndrome] and exercise your way to health is foolishness. It is insane. — Dr Paul Cheney
We’ve documented, as have others, that the level of functional impairment in people who suffer from CFS is comparable to multiple sclerosis, AIDS, endstage renal failure, chronic obstructive pulmonary disease. The disability is equivalent to that of some wellknown, very severe medical conditions. – Dr William Reeves
It’s amazing to me that anyone can look at these patients and not see that this is an infectious disease that has ruined lives. – Dr. Judy Mikovits
ME/CFS has a greater negative impact on functional status and well-being than other chronic diseases, e.g., cancer or lung diseases, and is associated with a drastic decrement in physical functioning. In a comparison study ME/CFS patients scored significantly lower than patients with hypertension, congestive heart failure, acute myocardial infarction, and multiple sclerosis (MS), on all of the eight Short Form Health Survey (SF-36) subscales. As compared to patients with depression, ME/CFS patients scored significantly lower on all the scales, except for scales measuring mental health and role disability due to emotional problems, on which they scored significantly higher. ― Frank Twisk
Every single medical person who is truly involved in the care of someone with ME acknowledges just how severely the illness impacts the sufferers and their families.
#8 : fear of missing outside the worse …
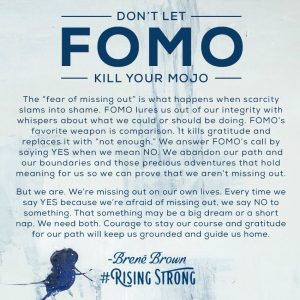
The actual fear of missing out (FOMO) is real and affects every single one of us, regardless of our health level or age.
But with illness, it’s a little more intricate. Because no one wants to keep saying no to invitations and spend their days and nights just lay in a darkened room missing out on living.
No one wants to feel guilty about not pulling their weight in their family setup.
No matter how much I love these words, (see image on the left), by Brené Brown, who so eloquently explains the problem of having a fear of missing out.
Yet, as someone who is severely sick and misses out on so much because of the illness it can hardly be so simple as staying the course.
You lost your mojo because of illness and you fear missing out not because you haven’t stayed strong and stayed the course. It’s because the illness is in control not your will power or determination.
#9 : when you don’t see me …
You will see me far less than you do see me and it is really important for you to know that when you don’t see me it’s because I am poorly.
And when you don’t see me for extended periods of time know that this means I am really struggling.
When thes things occur, because they will, …
Please help me realise that it’s okay not to be okay.
Help me accept that it’s all okay and that you will stick around no matter how long it takes me to …
#10 : I am not exaggerating …
I am not exaggerating when I say blah blah blah …
I feel like I am dying …
I have never had so much pain
I have never felt so poorly
When I think of death, and of late the idea has come with alarming frequency, I seem at peace with the idea that a day will dawn when I no longer be among those living in this valley of strange humors.
I can accept the idea of my own demise, but I am unable to accept the death of anyone else.
I find it impossible to let a friend or relative go into that country to no return.
Disbelief becomes my close companion, and anger follows in its wake.
I answer the heroic question ‘Death, where is thy sting?’ with ‘It is here in my heart and mind and memories. ~ Maya Angelou, When I Think of Death
… there are days when I am so poorly …
… I am scared I might be dying …
in summary & in conclusion …
These are just ten thing I wish you knew about ME buy there are thousands more I could have shared.
a personal concluding note …
For me the most important one has to be please believe me when I say blah blah blah …
Please feel free to contact me to share your outcomes or with any questions you may have.
fragmented.ME xXx




